Going Into the Hospital? What You Need to Know About Blood Clots
One in four people worldwide die from conditions related to thrombosis, the formation of clots in a blood vessel. Events related to thrombosis cause more deaths each year in the U.S. and Europe than breast cancer, HIV disease, and motor vehicle crashes combined, yet few people know about blood clots, or that they often have a surprising origin – the hospital.
Harmful blood clots typically form in the deep veins of the leg, groin or arm and are referred to as deep vein thrombosis (DVT). A DVT can then travel in the circulation system and lodge in the lungs, also known as a pulmonary embolism (PE). Together, DVT and PE are known as venous thromboembolism (VTE), a dangerous, and potentially deadly medical condition.
Being in the hospital is a major risk factor for the development of VTE. Patients with decreased mobility due to bedrest or recovery, or who experience blood vessel trauma due to surgery or other serious injury, are more likely to develop blood clots.
Hospital-associated thrombosis is a global problem. In a major study sponsored by the World Health Organization (WHO), it accounted for more deaths and disability than hospital-acquired pneumonia, catheter-related bloodstream infections, or adverse drug events in low and middle-income countries. It also accounts for up to 300,000 deaths in the U.S. and 544,000 deaths in Europe each year. In the U.K., however, figures have been falling over the last decade thanks to mandated VTE prevention measures instituted in hospitals by England’s National Health Service (NHS). Since 2010, England has seen a 15.4 percent reduction in deaths within 90 days after hospital discharge.
The example of NHS England in the U.K. shows that by focusing on hospital-associated VTE prevention, healthcare systems can save lives and reduce costs. According to a recent article in the British Medical Journal authored by Prof. Beverley Hunt, MD, OBE, and chair of the World Thrombosis Day Steering Committee, NHS England’s hospitals lowered their VTE rates significantly by implementing mandated patient risk assessments, adherence to guidelines, and investigation of cases to determine their root causes. In the U.S., Johns Hopkins Medicine reported a 40 percent reduction in VTE events after implementing a similar prophylaxis protocol.
While some hospitals and healthcare systems have adopted comparable measures for preventing VTE, that is not true everywhere. This means patients must be proactive in speaking with their care providers about the steps they can take to identify and prevent thrombosis. During their stay at the hospital and after being discharged, patients should be alert for signs and symptoms of thrombosis, such as leg pain and tenderness, redness and swelling, shortness of breath, rapid breathing, chest pain and coughing up blood.
Thrombosis survivor Scott Shields of Arlington, Virginia, says, “A car crash when I was 32 left me with multiple life-threatening injuries. But when I was recovering in the hospital, I developed a deep vein thrombosis (DVT) in my left thigh. Because I was communicating with my doctors daily during physical therapy sessions, I was able to bring their attention to this new, sudden pain in my leg, and get rapid treatment.”
As Shields indicates, an open line of communication with health care providers is essential. Patients should be able to expect that their hospital stay is safe and that the risk of adverse events such as blood clots is minimized, but they should also feel empowered to advocate for their own care.
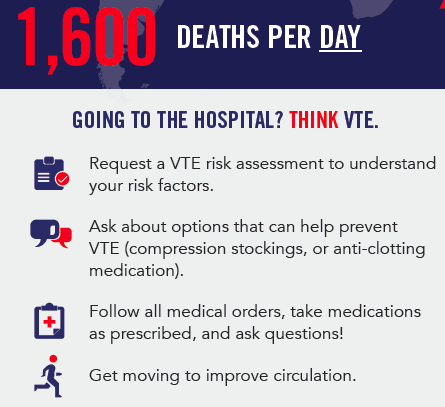
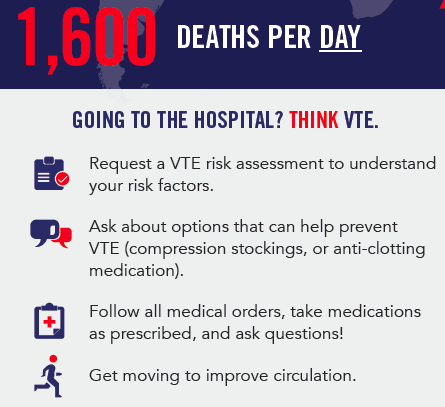
Hospitalized patients should take the following steps to help assess their risk and prevent VTE:
• Ask your provider for a VTE risk assessment, a tool or questionnaire that gathers information about a patient’s age, medical history, medications, and specific lifestyle factors to discern a patient’s potential risk for developing blood clots.
• Ask about treatment options like compression stockings or anti-clotting medication that can help prevent VTE.
• Follow prescribed treatments, including medication, as ordered, and ask questions if you have any.
• Stay active and moving as much as possible while in the hospital and after discharge.
For more information about blood clots, visit the World Thrombosis Day website. World Thrombosis Day is on October 13 each year and is led by the International Society on Thrombosis and Haemostasis (ISTH).
1 – Journal of Thrombosis and Haemostasis, “Thrombosis: A Major Contributor to Global Disease Burden,” (2016).
http://onlinelibrary.wiley.com/doi/10.1111/jth.12698/full
2 – American Heart Journal, “The Design and Implementation of a New Surveillance System for Venous Thromboembolism Using Combined Active and Passive Methods,” (2015).
www.cdc.gov/ncbddd/dvt/features/keyfinding-bloodclots-vte.html
3 – Hunt, B. (2019) Preventing hospital-associated venous thromboembolism. BMJ, 365, l4239.