Arterial Thrombosis: Causes, Symptoms, Prevention
What is Arterial Thrombosis?
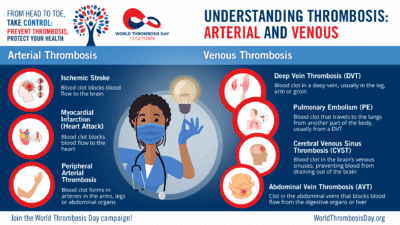
A blood clot within an artery is known as an arterial thrombosis. Arterial thrombosis is responsible for heart attacks, strokes and peripheral vascular disease (blood clot in arm or leg arteries). Arterial thrombosis typically occurs when there’s damage to the inner lining of an artery (the endothelium), often due to atherosclerosis (buildup of fatty plaques). When a plaque ruptures or becomes unstable, it triggers the blood clotting cascade, causing platelets to stick together and form a clot at that site.
Arterial thrombosis differs significantly from venous thrombosis. While arterial clots form in high-pressure vessels carrying oxygen-rich blood and develop rapidly, venous clots occur in low-pressure veins returning blood to the heart and typically form more slowly. Each type has distinct risk factors, symptoms and treatment approaches.
Understanding arterial thrombosis symptoms and seeking immediate medical attention can prevent permanent organ damage and save lives.
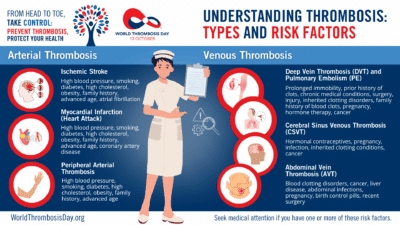
Arterial Thrombosis Risk Factors
Most arterial thrombosis cases result from atherosclerosis, a condition where fatty deposits, cholesterol and other substances accumulate inside artery walls. These buildups create plaques that can restrict blood flow or rupture, forming blood clots that completely block arteries.
The primary risk factors for arterial thrombosis match those for atherosclerosis. While specific risk factors exist for different arterial blockage types — including stroke, heart attack and peripheral artery disease — atherosclerosis plays a central role in all conditions. Managing atherosclerosis risk factors can reduce arterial thrombosis risk in most patients.


Controllable Risk Factors
While age and family history cannot be changed, many important atherosclerosis factors can be controlled, including high blood pressure, high cholesterol, smoking, diabetes, obesity and sedentary lifestyle.
Non-Atherosclerotic Causes
In some patients, arterial thrombosis occurs without atherosclerosis. Contributing factors include hypercoagulable disorders like antiphospholipid syndrome; inflammatory and autoimmune diseases such as lupus or severe infections; trauma or artery damage; atrial fibrillation, which can create heart clots that travel to the brain (causing stroke) or other arteries; and cancer or certain medications.
Non-Modifiable Risk Factors
Age remains the strongest predictor of arterial thrombosis, with risk increasing dramatically after age 50. Studies show exponential growth in both arterial and venous blood clot events as people age. Increased life expectancy in recent decades has contributed to the current rise in thrombosis cases.
Family history represents another crucial factor, closely linked to genetic risk factors that promote blood clotting. However, unlike venous blood clots where specific hereditary conditions are well-identified, scientists know less about genetic variations that increase arterial thrombosis risk. Doctors typically don’t order genetic testing for arterial blood clot patients.
Modifiable Risk Factors:
Modifiable Risk Factors:
- Smoking cessation can significantly reduce arterial thrombosis risk
- Blood pressure control through medication and lifestyle changes
- Cholesterol management with diet and medications when needed
- Diabetes management and blood sugar control
- Regular physical activity and weight management
- Limiting alcohol consumption


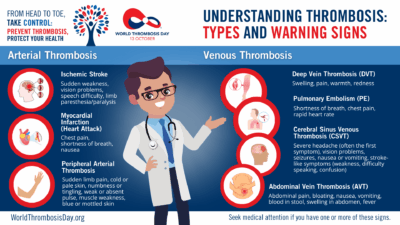
Recognizing Emergency Symptoms
Arterial thrombosis can cause life-threatening emergencies requiring immediate medical attention. Seek immediate medical attention if you experience:
Heart Attack Warning Signs:
- Chest pain or pressure lasting more than a few minutes
- Pain radiating to arms, neck, jaw or back
- Shortness of breath with or without chest discomfort
- Nausea, lightheadedness or cold sweats
Stroke Warning Signs:
- Sudden numbness or weakness in face, arm or leg
- Sudden confusion or trouble speaking
- Sudden vision problems in one or both eyes
- Sudden severe headache with no known cause
- Sudden trouble walking or loss of coordination

Research on Arterial Thrombosis from the International Society on Thrombosis and Haemostasis (ISTH)
- “Hypercoagulability and the risk of myocardial infarction and ischemic stroke in young women“ – Siegerink B, et al. J Thromb Haemost. 2015;13(9):1568-75. doi: 10.1111/jth.13045
- “Mortality due to bleeding, myocardial infarction and stroke in dialysis patients“ – Ocak G, et al. J Thromb Haemost. 2018;16(10):1953-1963. doi: 10.1111/jth.14254
- “Hand grip strength and risk of incident venous thromboembolism: The Tromsø study“ – Leknessund OGR, et al. Res Pract Thromb Haemost. 2022;6(7):e12833. doi: 10.1002/rth2.12833
- “Prevention of arterial and venous thrombotic events in symptomatic peripheral arterial disease patients after lower extremity revascularization in the VOYAGER PAD trial: Dual anticoagulant/antiplatelet regimen vs antiplatelet therapy alone” – Berkowitz SD, et al. J Thromb Haemost. 2022;20(5):1193-1205. doi: 10.1111/jth.15673
- “No prospective association of a polygenic risk score for coronary artery disease with venous thromboembolism incidence” – Folsom AR, et al. J Thromb Haemost. 2021;19(11):2841-2844. doi: 10.1111/jth.15501
- “Pharmacological targeting of coagulation factor XI mitigates the development of experimental atherosclerosis in low-density lipoprotein receptor-deficient mice” – Ngo ATP, et al. J Thromb Haemost. 2021;19(4):1001-1017. doi: 10.1111/jth.15236
- “The coagulation system in atherothrombosis: Implications for new therapeutic strategies” – Olie RH, et al. Res Pract Thromb Haemost. 2018;2(2):188-198. doi: 10.1002/rth2.12080
- “Genome-wide association study validation identifies novel loci for atherosclerotic cardiovascular disease” – Chen X, et al. J Thromb Haemost. 2012;10(8):1508-1514. doi: 10.1111/j.1538-7836.2012.04815.x
Page references:
https://www.nhs.uk/conditions/arterial-thrombosis/
American Heart Association. (2024). Heart Disease and Stroke Statistics: A Report of US and Global Data. Circulation, 149(8), e347-e913. doi: 10.1161/CIR.0000000000001209
Ocak G, Noordzij M, Rookmaaker MB, et al. (2018). Mortality due to bleeding, myocardial infarction and stroke in dialysis patients. Journal of Thrombosis and Haemostasis, 16(10), 1953-1963. doi: 10.1111/jth.14254
Previtali E, Bucciarelli P, Passamonti SM, Martinelli I. (2011). Risk factors for venous and arterial thrombosis. Blood Transfusion, 9(2), 120-138.
Siegerink B, Maino A, Algra A, Rosendaal FR. (2015). Hypercoagulability and the risk of myocardial infarction and ischemic stroke in young women. Journal of Thrombosis and Haemostasis, 13(9), 1568-75. doi: 10.1111/jth.13045